Can Menopause Cause High Blood Sugar? The Truth Revealed
The answer to the question of how menopause affects blood sugar is complicated. There are a variety of factors that can contribute to high sugar levels, including age, weight, diet, and genetics.
Table of Contents
ToggleMenopause itself doesn’t cause high blood glucose levels, but the hormonal changes associated with menopause can lead to insulin resistance.
Then, of course, your body has a harder time using insulin to move glucose from your bloodstream into your cells. As a result, the level of sugar may rise.
Also, some common symptoms of menopause can also increase your blood sugar.
Causes of High Blood Sugar in Menopause
Hormonal Changes
A few things happen during menopause that might lead to higher blood sugar levels. One of these is the decrease in the hormone estrogen.
Estrogen helps keep your blood glucose in check by increasing the sensitivity of your cells to insulin. When the amount of estrogen your body produces drops, it commonly leads to insulin resistance and higher blood sugar levels as a result.
Another hormonal change that happens during menopause is an increase in cortisol, the stress hormone. This hormone has a number of different effects on your body, one of which is to raise the amount of sugar in the blood.
Cortisol helps break down glycogen (a stored form of glucose), so it can be released into the bloodstream. As such, additional cortisol is associated with sudden spikes in blood sugar.
Another sex hormone that is reduced during menopause is progesterone. There is no clear answer as to whether low amounts of progesterone can increase sugar levels in menopause. More research is needed in order to determine if there is a definite connection.
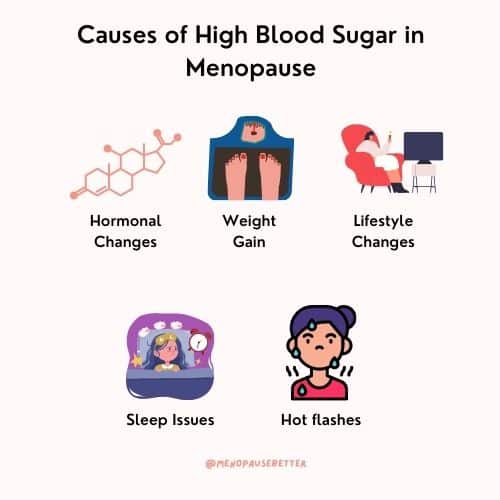
Weight Gain During Menopause
One of the issues facing menopausal women is weight gain, which can also raise the amount of glucose in the blood. The weight gain that occurs during menopause is often multifactorial.
Because of the hormone imbalance related to menopause, it becomes easier for your body to store fat and lose muscle mass. It’s also easier to build up fat in the abdomen, called visceral fat or stress belly.
Abdominal fat is another symptom of menopause that increases the risk of insulin resistance and high blood glucose.
Lifestyle Changes
Weight gain is not the only reason why menopausal women may have higher blood glucose. It is also common for women to experience a change in their eating habits during menopause.
Many women find that their appetite decreases, and they start to crave sugary and fatty foods. Also, many women change their physical activity levels during menopause.
Both can lead to weight gain and, as a result, higher blood sugar levels.
Sleep Issues
Many women experience a lack of sleep or poor sleep during menopause.
According to the sleep foundation, even partial sleep deprivation can increase insulin resistance, which in turn increases blood sugar levels. What’s more, poor sleep can:
- Result in higher cortisol levels, which increases glucose
- Increase the growth hormone that raises blood sugar during sleep
- Result in higher oxidative stress, which also impacts glucose levels
- Elevate inflammatory markers, which can cause insulin resistance
Additionally, when you don’t get enough sleep, your body produces the hormone ghrelin, also known as the “hunger hormone.” This can cause you to eat more, leading to weight gain, which is also a risk factor for diabetes.
Hot Flashes
Science backs up anecdotal stories about how high blood glucose and insulin resistance are linked to hot flashes, one of the most widespread menopause symptoms.
For example, a study has shown that women who reported hot flashes frequently had glucose levels 33% higher than those reporting no hot flashes.
Another study suggests that hot flashes, especially when accompanied by night sweats, can lead to diabetes.
Complications of High Blood Glucose
High blood sugar can lead to a number of health problems, including:
- Diabetes
- Hot flushes
- Heart disease
- Stroke
- Kidney disease
- Eye damage
- Nerve damage
- Skin problems
- High blood pressure
- Metabolic syndrome
What Are Normal Blood Sugar Levels?
The American Diabetes Association says that normal blood glucose is measured as:
Fasting: less than 100 mg/dL
Random or post-meal: less than 140 mg/dL
A normal result for A1C (a test that measures blood sugar over three months) is below 6%
Tips to Lower Blood Sugar
There are a number of things that you can do to lower your blood sugar levels if they are high. Here are some easy changes you can make to improve the amount of glucose in your blood.
Eat a Healthy Diet
There are a few simple ways to eat healthily and prevent high blood sugar. First, choose complex carbohydrates over simple sugars. Complex carbs are slowly absorbed by the body, which helps to keep sugar levels from spiking.
Second, eat plenty of fiber-rich foods. Fiber also helps to control glucose levels by slowing down digestion.
Third, include healthy fats in your diet. Healthy fats help to regulate insulin, which can prevent both high and low blood sugar.
Last, have an overall healthy diet with a good balance of vegetables, fruits, lean protein, complex carbohydrates, and healthy fats.
The healthy eating plate or the USDA plate can quickly provide can help you follow a healthy diet.

Exercise Regularly
When you exercise, your muscles use glucose for energy. This can cause your blood sugar level to drop temporarily. However, over time, regular exercise can help to lower it permanently.
Exercise also helps to improve insulin sensitivity. This means that your body will be better able to use it to control blood sugar. Insulin resistance is a major cause of problems in this regard.
By improving insulin sensitivity, you can effectively lower your blood sugar level.
Lose Weight
Did you know that losing weight can help reduce high levels of glucose in the blood? In fact, research has shown that even a modest amount of weight loss can make a big difference.
One reason is that when you’re carrying excess weight, your body produces more insulin to control the sugar levels in your blood. Over time, this tends to lead to insulin resistance, a major factor in type 2 diabetes.
But as we all know, weight loss is not always easy, especially once menopause hits. That’s why it’s important to talk to your doctor or a registered dietitian who can help you develop a plan that’s right for you. They can also offer tips and support to help you stay on track.
Reduce Stress
As we have seen, there are many factors that influence the amount of sugar in the blood, but one of the most powerful is stress. When we experience stress, our body releases cortisol.
Cortisol can increase the amount of glucose in the blood, which can eventually lead to diabetes. Therefore, it’s important to find ways to reduce stress in your life in order to keep this at a healthy level.
Keep Hydrated
Drinking plenty of water is one healthy habit that can make a big difference.
Drinking water helps to keep your kidneys functioning properly. As they also play an important role in regulating blood sugar, it’s important to keep them healthy.

Nutrition Supplements to Lower Blood Sugar
Magnesium
Magnesium helps to control glucose in the blood by improving insulin sensitivity and thereby regulating the level.
Furthermore, magnesium is also involved in metabolizing glucose, helping to convert it into energy. Studies have shown that magnesium deficiency is linked to both type 2 diabetes and prediabetes.
As a result, Including magnesium-rich foods in your diet or taking a magnesium supplement may help to prevent high blood sugar.
Foods high in magnesium include leafy green vegetables, nuts, seeds, and beans. It’s also found in some fruits, like bananas and avocados.
If you’re considering a magnesium supplement, you might be interested in reading more about menopause and magnesium.
Zinc
Zinc is another mineral that plays a role in controlling the amount of sugar in the blood. Like magnesium, zinc helps to regulate insulin and improve sensitivity. It’s also involved in glucose metabolism and has shown improvement in people with diabetes.
Good sources of zinc include meat, poultry, beans, seafood,, nuts, and seeds. It’s also found in some fortified foods, such as breakfast cereals and milk.
Cinnamon
Cinnamon is a common spice that is popular in helping to control blood sugar. It contains a compound called cinnamaldehyde, which has been proven to improve insulin sensitivity and help regulate sugar in the blood.
In addition, cinnamon also slows the emptying of the stomach, which can help to control blood glucose after a meal.
You can easily add cinnamon to your diet by sprinkling it on top of oatmeal or yogurt or adding it to smoothies or baked goods.
The Bottom Line
Can menopause cause high blood sugar? The truth is yes, it can, but there are ways to prevent it.
Most people are able to keep their blood sugar level under control by eating a healthy diet, exercising regularly, reducing stress, drinking plenty of water, and maintaining a healthy body weight.
However, for some people, lifestyle changes are not enough, and they require medication. If you suspect you have high blood glucose, it’s best to consult with your healthcare team who will create a treatment plan to work well for you.
References
Cortisol. Wikipedia. https://en.wikipedia.org/wiki/Cortisol#:~:text=Cortisol%20also%20plays%20an%20important,action%20of%20glucagon%20and%20adrenaline. Published June 1, 2022. Accessed July 2, 2022.
Diagnosis. Diagnosis | ADA. https://www.diabetes.org/diabetes/a1c/diagnosis. Accessed July 3, 2022.
Escobar S-N. Good night’s sleep is the key to health and happiness. Menopause Better. https://menopausebetter.com/good-nights-sleep-is-the-key-to-health-and-happiness/#Sleep_and_Insulin_Resistance. Published April 21, 2022. Accessed July 2, 2022.
Herber-Gast G-CM, Mishra GD. Fruit, Mediterranean-style, and high-fat and -sugar diets are associated with the risk of night sweats and Hot Flushes in midlife: Results from a prospective Cohort Study. The American Journal of Clinical Nutrition. 2013;97(5):1092-1099. doi:10.3945/ajcn.112.049965
Hot flashes could be precursor to diabetes, study suggests. ScienceDaily. https://www.sciencedaily.com/releases/2017/12/171206090537.htm. Published December 6, 2017. Accessed July 2, 2022.
Lowry F. Hot flashes linked to insulin resistance. Medscape. https://www.medscape.com/viewarticle/772465#vp_2. Published July 26, 2020. Accessed July 2, 2022.
Morselli L, Leproult R, Balbo M, Spiegel K. Role of sleep duration in the regulation of glucose metabolism and appetite. Best Practice & Research Clinical Endocrinology & Metabolism. 2010;24(5):687-702. doi:10.1016/j.beem.2010.07.005
Sleep & glucose: How blood sugar can affect rest. Sleep Foundation. https://www.sleepfoundation.org/physical-health/sleep-and-blood-glucose-levels#:~:text=Decreased%20sleep%20is%20a%20risk,diabetes%2C%20a%20blood%20sugar%20disorder. Published April 1, 2022. Accessed July 3, 2022.
Yan H, Yang W, Zhou F, et al. Estrogen improves insulin sensitivity and suppresses gluconeogenesis via the transcription factor FOXO1. Diabetes. 2018;68(2):291-304. doi:10.2337/db18-0638

Dr. Su-Nui Escobar, a Registered Dietitian/Nutritionist in Miami, FL, is dedicated to empowering women in perimenopause and menopause to live healthier, more satisfying lives.
With a doctorate in clinical nutrition from the University of North Florida, she has expertise in menopause and weight loss, including the unique challenges faced by those on weight loss medications.
Su-Nui’s passion for her field is evident in her previous role as the Academy of Nutrition and Dietetics spokesperson.