What Menopause Means for Your Digestion
Did you know that menopause can also affect your digestive system? If you’re experiencing GI difficulties such as constipation, abdominal bloating, diarrhea, or stomach pain, you can blame hormonal fluctuations!
Table of Contents
ToggleThis article explores the link between menopause and digestion. Most important, it touches upon what to do about it.
Menopause Constipation
Menopause constipation is a common menopausal symptom. During this stage in every woman’s life, the estrogen and progesterone levels decrease, leading to changes in bowel movements in some women (1).
Other hormonal imbalances during menopause can also contribute to this problem. For example, some imbalances in the hormones that maintain the body’s fluid balance can cause constipation by retaining fluids (water retention). As a result, the food bolus will compact and dry out, and a dry bolus will take longer to travel through the intestine (2).
Tips to Manage Constipation
Healthy Eating
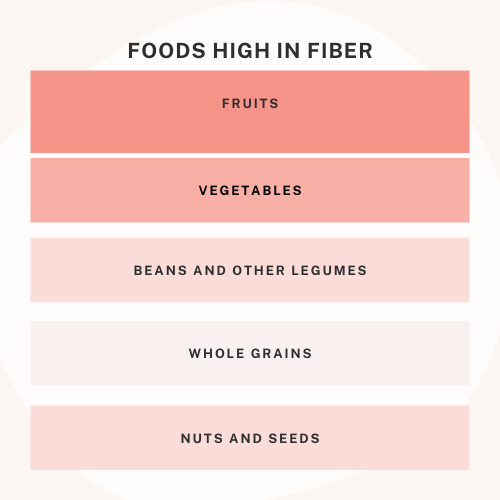
The obvious change to decrease constipation is to eat a fiber-rich diet that includes fruits and vegetables, whole grains, and legumes (such as beans and lentils).
Drink Plenty of Fluids
Dehydration and constipation go hand in hand. Keep your body hydrated, and you should notice an improvement in menopause constipation.
Increase Your Physical Activity
Regular exercise decreases menopause constipation by stimulating blood circulation, strengthening the pelvic floor or abdomen muscles, increasing muscle tone throughout the colon, and regulating intestinal contraction times.
A gentle form of yoga called restorative yoga is helpful for menopause constipation because it promotes relaxation while stretching and lengthening both abdominal and lower back muscles.
Manage Stress Level
In this stage of a woman’s life, the decrease of the sex hormones results in an imbalance of the stress hormone cortisol. As a result, stress can easily overwhelm the GI tract, leading to various digestive issues.
Adjusting Your Medication Dosages
If you are on certain over-the-counter or prescription medications such as antidepressants or antacids, talk with your doctor about whether a change in dose may help relieve menopause constipation.
Medications and Constipation
If you are still struggling with menopause constipation after making lifestyle changes, it could be time for short-term use of laxatives.
However, if the problem persists, it is worth talking to your doctor.
Menopause and Diarrhea
Menopausal women often experience bouts of diarrhea. This is mainly due to changes in hormone levels leading to intestinal permeability -leaky gut (3), causing diarrhea by irritating the lining of your digestive tract, weakening stomach muscles, or reducing the absorption of food into the body.
That being said, it is important to recognize that two types of menopause diarrhea are typically experienced – chronic and acute.
Acute diarrhea is most common in the first three months following menopause, and chronic diarrhea is most common after six to 12 months.
Diarrhea can also be related to other conditions such as irritable bowel syndrome, irritable bowel disease, Crohn’s disease, and gallbladder problems.
Therefore finding the cause of diarrhea is essential, especially if diarrhea is a symptom that continues after making lifestyle changes.
Tips to Manage Diarrhea
Drink Plenty of Fluids
Mostly, this is important to prevent dehydration.
Eat Soluble Fiber
It sounds weird, but soluble fiber can help form the stool.
Foods containing soluble fiber include oats, beans, sweet potatoes, broccoli, carrots, pears, figs, nectarines, apricots, apples, flaxseeds, sunflower seeds, and hazelnuts.
Reduce Stress Levels
Stress and gut health have a strong connection. When you experience chronic stress, there is a cascade of negative effects on your digestive process (4).
Thus, by managing stress, you can improve gut health while improving many other symptoms of menopause.
New Food Intolerances
Foods that you tolerated well before now may be more difficult for you to digest. For example, gluten and lactose intolerance are common in many adults. So, be aware of what you eat, and if you notice that certain foods cause diarrhea, eliminate them for a few weeks. Then, you can re-introduce these foods later and see how you feel.
Probiotics
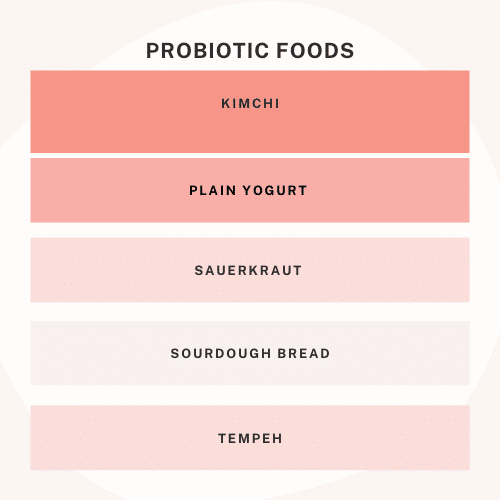
Probiotics have special microorganisms that can fight the germs that cause diarrhea (5). They are so effective that they quickly became a standard treatment for hospitalized patients with diarrhea.
These supplements are both gentile and beneficial for your overall health. For example, probiotics can also strengthen your immune system by protecting the gut.
Good sources of probiotics include yogurt, kefir, tempeh (fermented soy), miso soup, sauerkraut, kimchi, olives, pickles, and many others.
The more fermented food is – the better source it will be because the time spent fermenting makes an already nutrient-rich food even healthier by promoting colonization with health-promoting microorganisms.
Beyond eating foods high in probiotics, taking supplements can be good for your digestive health.
Seek Medical Health
If diarrhea continues, it is time to seek medical help to determine the underlying cause of the problem. Diarrhea is often a symptom of a problem, not a problem by itself.
The doctor will usually perform a physical exam to determine if a menopausal woman has a functional or organic condition causing menopausal diarrhea.
If an organic cause for diarrhea is found, your physician might prescribe medication.
If an organic cause for menopause diarrhea cannot be identified or if no treatment relieves symptoms, the doctor may recommend an endoscopic evaluation to identify any structural abnormalities of the gastrointestinal tract that could contribute to menopause diarrhea.
Menopause Gallbladder Problems
Menopausal women have an increased risk of developing gallbladder disease.
This is due to changes in hormone levels which can weaken your stomach muscles and increase intestinal permeability (leaky gut), leading to inflammation in the bile ducts.
A malfunctioning gallbladder can result in abdominal pain after eating, nausea, bloating, and indigestion.
It is important to speak to your physician if you believe your gallbladder is not working properly.
Menopause Nausea
Menopausal women often experience nausea, mainly due to hormonal changes that weaken stomach muscles, increase intestinal permeability (leaky gut) and lead to inflammation in the bile ducts. As mentioned before, this can cause nausea.
Tips to Relieve Nausea
Drink ice-cold drinks
Drink beverages slowly
Eat small, frequent meals
Avoid heavy foods
Avoid foods high in fat
Eat cold meals
If nausea persists, seek medical help to find the root cause.
Conclusion
While there are many possible causes of digestive problems, menopause is a common culprit. However, nutrition and lifestyle changes can make a big difference; it is always amazing how simple changes go a long way!
What are your thoughts on this? Have you experienced any of these digestive issues while going through menopause or after experiencing the change in hormone levels? We’d love to hear about it. Leave us a comment below!

Dr. Su-Nui Escobar, a Registered Dietitian/Nutritionist in Miami, FL, is dedicated to empowering women in perimenopause and menopause to live healthier, more satisfying lives.
With a doctorate in clinical nutrition from the University of North Florida, she has expertise in menopause and weight loss, including the unique challenges faced by those on weight loss medications.
Su-Nui’s passion for her field is evident in her previous role as the Academy of Nutrition and Dietetics spokesperson.