The Connection Between Perimenopause and Stomach Issues
Experiencing perimenopause stomach problems is stressful and unpleasant.
Table of Contents
ToggleTransitioning into perimenopause can bring about digestive problems or make existing stomach issues worse. However, there is good news; stomach problems are fixable through diet and lifestyle changes.
This article will discuss the causes and treatment options for perimenopause stomach problems.
What are Perimenopause Stomach Problems?
Stomach problems are common and may impact not only the stomach, but also the small or large intestine. In perimenopause, female sex hormones play a role in digestive issues. Specifically, estrogen and progesterone hormones responsible for the menstrual cycle frequently impact the digestive tract, worsening stomach issues. (1)
Stomach Problems Symptoms
Women with stomach issues might experience any of the following symptoms. (2)
- Constipation
- Diarrhea
- Bloating
- Abdominal pain
- Abdominal cramping
- Gas
- Belching
- Heartburn
- Gastroesophageal reflux
- Nausea
- Vomiting
- Indigestion
Who gets Perimenopause Stomach Problems?
Perimenopause is the period when your body begins transitioning into menopause. This can occur in women as early as their mid-30s to as late as their 50s. Along with typical perimenopause symptoms, women may also develop digestive problems.
Women in perimenopause experience changes in the ovarian hormones estrogen and progesterone. Throughout perimenopause, estrogen and progesterone rise and fall erratically. As a result, these changes in ovarian hormones affect and worsen symptoms of stomach issues.
If you are perimenopausal, the following risk factors set you up for stomach problems (3).
- Eating an unhealthy diet
- Having a family member with stomach issues
- A history of stressful or difficult life events
- Having a severe infection in the digestive tract
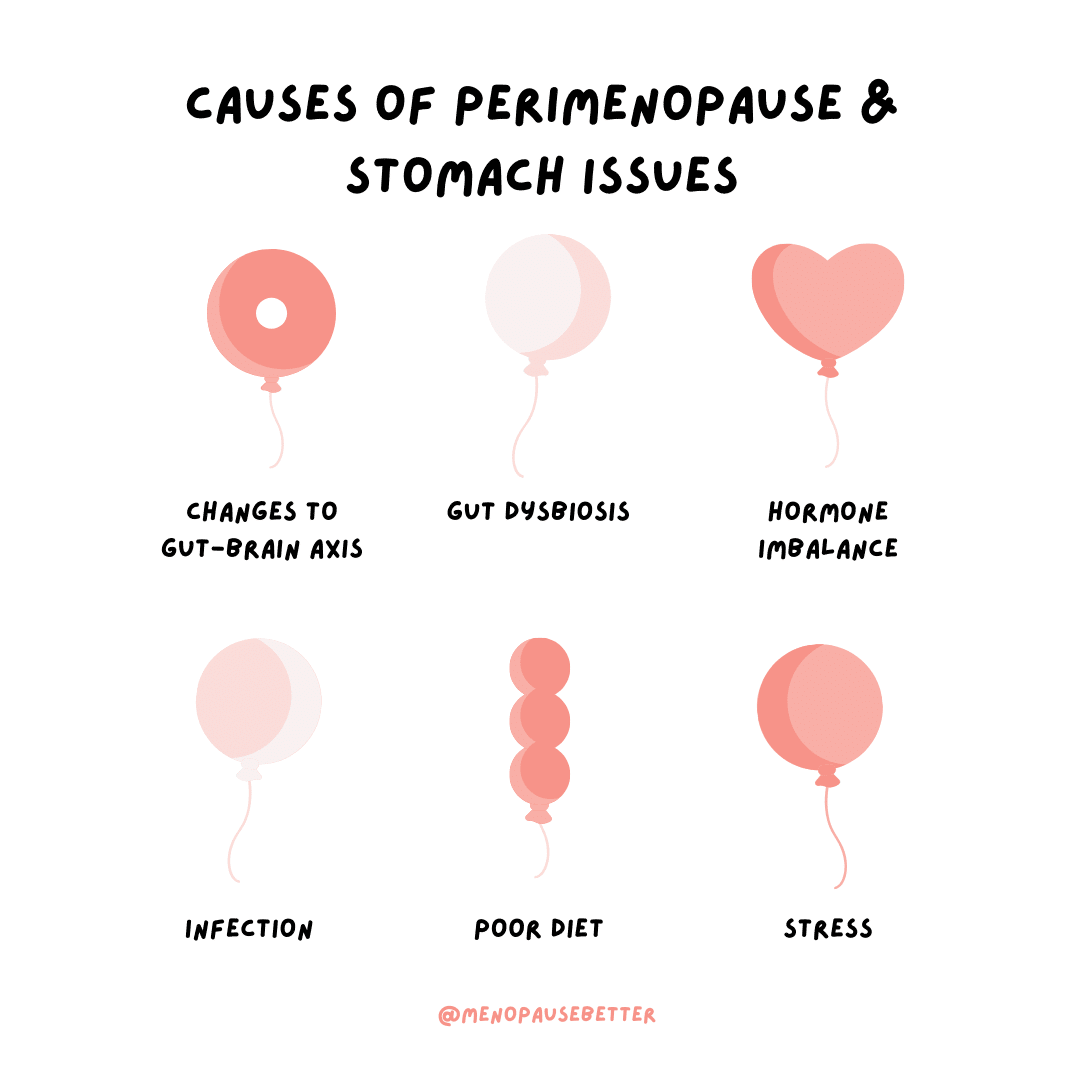
Causes of Perimenopause Stomach Problems
Many factors can impact the digestion of a perimenopausal woman.
Antibiotic Use
Antibiotics enable recovery from illness by killing harmful bacteria in your body. However, in the process, antibiotics also destroy the good bacteria that keep your digestive health in balance. As a result, many people suffer from diarrhea, cramping, and gas during antibiotic use. (4)
Taking probiotics along with antibiotics can help lessen the damage antibiotics cause to the stomach.
Bacterial, Viral, or Parasitic Infection
Infections from poor sanitation or unsafe water can create digestive problems. Common symptoms include stomach cramps, bloating, nausea, and diarrhea. (5)
Changes in the Gut-Brain axis
The brain interacts with the gut through neural and gastrointestinal components on a communication channel known as the gut-brain axis. Because of this, the brain can impact the gut microbiota, intestinal barrier, and intestinal immune response. (6)
Studies show that changes to the gut-brain axis can create digestive issues, specifically those found in irritable bowel syndrome (IBS).
Changes in Stomach Acid
Individuals can experience digestive issues when stomach acid leaves the stomach and enters into the esophagus. This is known as gastric reflux, which can cause common, symptoms like heartburn, nausea, or indigestion.(7)
Dysbiosis of Gut Microbiome
During perimenopause, you may experience gut dysbiosis. Dysbiosis is the condition of having an imbalance in the microbial community in the digestive tract. Medications, diet, and stress can all cause dysbiosis. Common symptoms of dysbiosis include diarrhea, constipation, nausea, abdominal bloating, and abdominal cramping. (8)
Food Intolerances
Food intolerance is typified by difficulty digesting certain foods and having an unpleasant physical reaction to them. Symptoms such as bloating, diarrhea, and constipation usually occur a few hours after eating the food you’re intolerant of. (9)
Common food intolerances include gluten, dairy, histamines, fructose, sucrose, and the short-chain carbs called FODMAPs that are resistant to digestion.
Changes to Digestive Motility
Declining levels of estrogen and progesterone slow digestive motility. As a result, food takes longer to get through your GI tract. The longer food remains in your digestive tract, the more water is reabsorbed back into your body. This reduction in water in your GI tract results in hard stools and constipation. Changes in hormone levels can also lead to intestinal permeability. This causes diarrhea by irritating the lining of your digestive tract, weakening stomach muscles, and reducing absorption of food into the body. (10)
Changes to Diet
Eating a diet low in plant foods can contribute to stomach issues. Fruits and vegetables are rich in fiber and prebiotics, which help digestion and support good gut bacteria. A diet high in processed foods, fast foods, and unhealthy fats will contribute to digestive issues and worsening gut bacteria. (11)
Increase in Pain Sensations
The estrogen hormone is associated with the production of serotonin, the feel-good hormone. During perimenopause, estrogen levels may drop, leading to decreased pain tolerance. As a result, abdominal pain associated with stomach issues may feel more painful. (12)
Increase in Cortisol Hormone
As women approach menopause, their levels of estrogen may increase, which can, in turn, increase the amount of cortisol. Having high cortisol in your system can negatively impact the digestive system, worsening gastrointestinal symptoms. (13)
Decrease in Bile Production
Low estrogen will also affect the production and flow of bile, which is key for digesting fats. When your body isn’t producing enough bile, your gut has trouble breaking down fats, often causing diarrhea.
Thus, women in perimenopause may be more sensitive to fat from food.
At the same time, in those with stomach issues, too much fat can activate pancreatic hormones, resulting in constipation. Thus, in addition to causing diarrhea, too much fat may also make symptoms like constipation worse. All in all, women who have perimenopause and stomach issues will likely experience problems digesting fat. This leads to worsening stomach issues. (14)
Increase in Sleep Disturbances
Sleep disturbances are a common occurrence during perimenopause.
During perimenopause, estrogen and progesterone levels fluctuate, leading to changes in cortisol and serotonin metabolism in the body. Cortisol and serotonin both help to regulate the body’s sleep cycle, so these changes will impact your ability to fall asleep and stay asleep..
Additionally, it is likely that a woman in perimenopause will experience hot flashes, which are also due to fluctuating hormones. You are likely to wake up right before experiencing a hot flash.Studies have shown that poor sleep is correlated to gastrointestinal diseases and worsening stomach issues. (15)
Diagnosing Perimenopause and Stomach Issues
Perimenopause is a natural part of life, so it is nots usually diagnosed. Women receive a diagnosis only if they are experiencing significant related discomfort.
Stomach issues will normally clear up on their own with proper diet and lifestyle changes.
However, if digestive problems persist over several months or don’t improve with a healthier diet and lifestyle, it’s important to visit a gastroenterologist to rule out any complex health issues.
Remedies for Perimenopause and Stomach Issues
There are a variety of ways to improve symptoms of perimenopause and digestive issues.
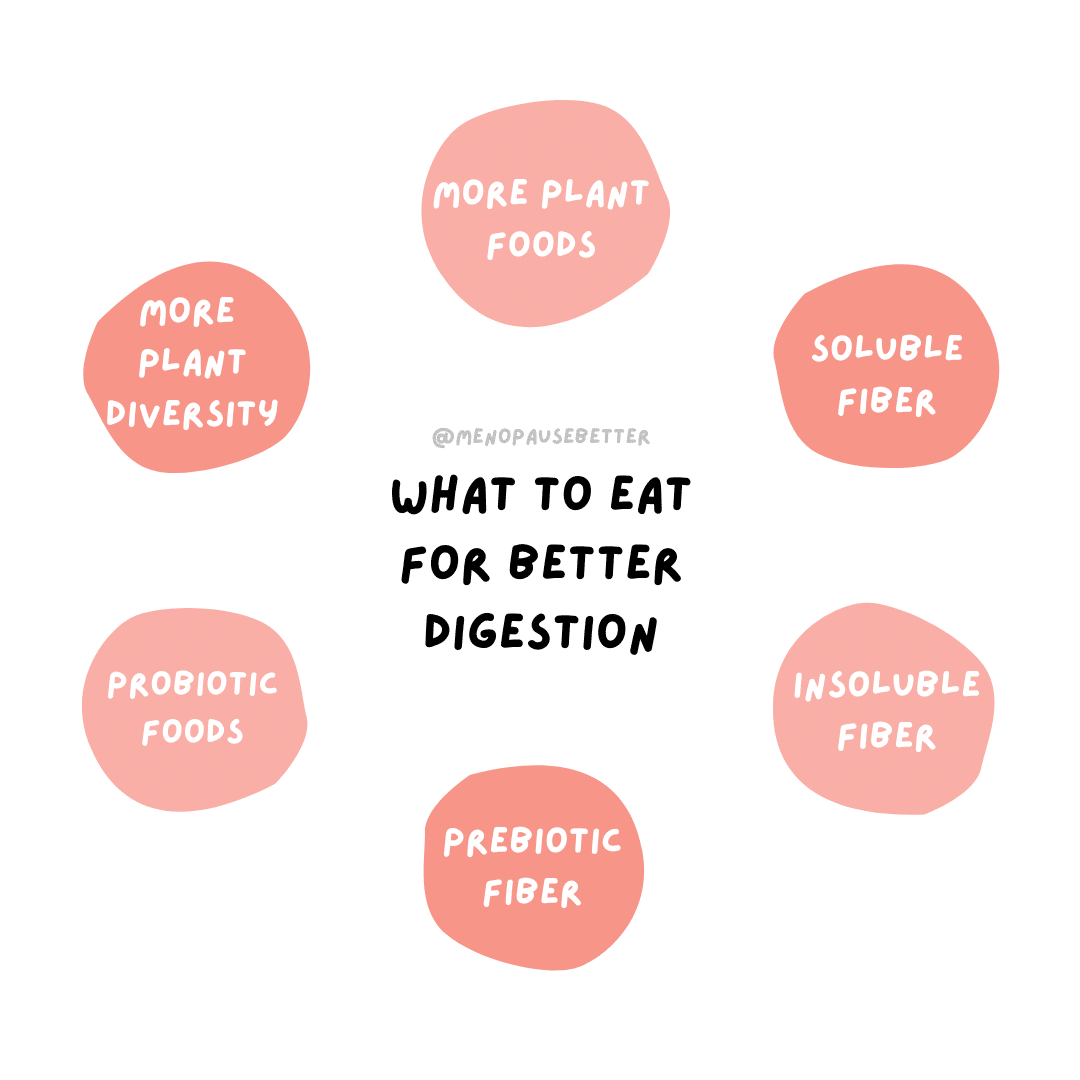
Change Fiber Intake
Including an appropriate amount of fiber in your diet can help manage your stomach issues.
Constipation: women will want to meet or exceed their fiber goals. It is particularly beneficial to add more insoluble fiber to your diet.
For example, insoluble fiber includes oranges, kiwis, raspberries, and brown rice.
Diarrhea: women will want to meet, but not exceed, their fiber goals. In addition, people with this problem will benefit from switching to more soluble fiber.
Examples of foods high in soluble fiber include oats, flax seeds, potatoes, and strawberries. (16)
Increase Plant Food
Plant foods like vegetables, fruits, nuts, seeds, and grains all contain digestion-friendly properties like fiber. Fiber helps regulate the digestive system.
A certain type of fiber called prebiotic fiber creates short-chain fatty acids (SCFAs) in the colon as a byproduct. SCFAs help nourish good gut bacteria, which supports digestive health and improves hormone balance. (17)
Foods with high amounts of SCFAs include garlic, onion, artichokes, leeks, wheat, apples, and potatoes.
Additionally, each plant food has its own microbiome. When you eat different varieties of plant foods per week, you take in a variety of healthy bacteria that improve your gut microbiome. (18)
Finally, eating probiotic foods like kefir, yogurt, miso, and sauerkraut also supports a healthy gut microbiome. A healthier gut microbiome enhances our digestive symptoms and balances hormones. (19)
Eat Smaller Meals
Eating smaller meals can help the digestive tract do its job. Eating large meals can result in too much pressure on the digestive tract that can create digestive issues.When you’re aiming to eat smaller meals, it helps to be aware of any tendencies to snack when you’re not hungry, to regulate portions when eating from large buffets, or the impulse to eat emotionally.
In addition, working on eating intuitively and acknowledging hunger and fullness cues can help regulate your eating patterns and quantities. (20)
Manage Fat Intake
Too much dietary fat can cause diarrhea or constipation if you have digestive problems.
Here are some easy tips for reducing fat intake::
- Cook food at home
- Reduce consumption take-out food
- Reduce consumption of packaged foods
- Avoid fast food (21)
Decrease Stress
Cortisol is called the ‘stress hormone’ because the body over-produces it when you are under pressure. As we have already seen, increases of cortisol can also affect estrogen, further worsening stomach symptoms. (22)
There are many ways to remedy stress and boost mental health. For example:
- Going on walks
- Spending time in nature
- Journaling
- Spending time with friends and family
- Playing with a pet
- Working on a hobby
- Yoga
- Pilates
- Practicing mindfulness
- Talk therapy
- Massage therapy
Increase Exercise
Exercise is an excellent way to decrease stress-related digestive issues. (23) Exercise increases blood flow throughout the body, including to the muscles that control digestion. This results in a decrease in constipation and bloating.
Furthermore, exercise can improve gut motility.
It’s important to find a type of exercise you enjoy. For example, take a 20-minute walk, do yoga, pilates, run, or participate in sports. The most important part of an exercise routine is consistently showing up.
Improve Sleep Quality
Poor sleep quality leads to worsening stomach issues and symptoms. The good news is that you can also improve the quality of your sleep by making diet and lifestyle changes. (24)
Some ways to improve sleep quality include:
- Keep bedroom at a cool temperature
- Wear sweat-wicking pajamas and sheets
- Go to bed and wake up at the same time every day
- Keep your bedroom dark
- Avoid large meals before bedtime
- Avoid drinking alcohol
- Exercise during the day
- Manage stress more effectively
- Avoid caffeine after the morning
Limit Alcohol
Limiting alcohol during perimenopause is a good idea for a variety of reasons.
First, drinking alcohol can increase estrogen levels, making stomach issues and symptoms worse. Furthermore, alcohol disrupts rapid eye movement (REM) sleep, which is the part of sleep that is the most restorative. Disrupted sleep leads to feeling tired the next day and being more likely to make poor health choices (25)
For instance, try replacing your nighttime wine or cocktail with a delicious mocktail, non-alcoholic beer, or a cup of warm caffeine-free tea.
Medications for Perimenopause and Stomach Issues
In some cases, diet and lifestyle may not be enough to manage your stomach issues. Therefore, other treatments such as over-the-counter and prescription medications are available to alleviate your symptoms.
Over the Counter
- Laxatives: increase transit time, relieving constipation or bloating
- Bulking agents: psyllium husk or bran can improve constipation, diarrhea, or bloating
- Herbs: peppermint or ginger tea can help with nausea and indigestion
Prescription
Sometimes prescription medications are necessary for the symptoms of more severe stomach issues. (26)
For example:
- Secretagogues/prosecretory drugs – increase fluid and movement in the GI tract
- Anticholinergics/antispasmodics – relieve abdominal pain or discomfort after eating
- Anti-diarrheal drugs – slow gut transit and decrease diarrhea
- Anti-anxiety medications – relieve pain and improve the changes in bowel habit
- Antidepressants – can reduce the intensity of pain signals going from gut to brain
Hormone replacement therapy (HRT) – helps balance hormones to improve digestion (27)
When When to See a Doctor About Perimenopause and Stomach Issues
Routine checks with your gastroenterologist will aid in managing stomach issues. However, there are times when a visit to your physician might be necessary in between these visits.
If stomach issues continue for months, or you experience any of the following symptoms, it’s important to see a doctor right away.
Symptoms include:
- Blood in your stool
- Hemorrhoids
- Unexplained weight loss
- Excessive gas
- Heartburn
- Chronic bloating
These symptoms might indicate a more chronic issue, such as irritable bowel syndrome (IBS), inflammatory bowel disease (IBD) or colon cancer. (28)
Summary
While perimenopause is a natural part of a woman’s life cycle, the addition of stomach problems may come as a shock. Changes in estrogen and progesterone may lead to worsening stomach issues symptoms, such as constipation, diarrhea, bloating, pain, nausea, or vomiting.
Digestive problems can be managed at home through various natural remedies, such as diet changes, exercise, better sleep, and stress reduction.
Additionally, you can speak to your doctor and health care team about taking prescription medication, if necessary.
In conclusion, always be sure to speak to your doctor if your symptoms are not improving over time.
Please share with those in your life that can benefit from reading this post.
“Perimenopause and Stomach issues” was written by Registered Dietitian Becky Rashidifard. Reviewed/edited by Su-Nui Escobar, DCN, RDN, FAND

Dr. Su-Nui Escobar, a Registered Dietitian/Nutritionist in Miami, FL, is dedicated to empowering women in perimenopause and menopause to live healthier, more satisfying lives.
With a doctorate in clinical nutrition from the University of North Florida, she has expertise in menopause and weight loss, including the unique challenges faced by those on weight loss medications.
Su-Nui’s passion for her field is evident in her previous role as the Academy of Nutrition and Dietetics spokesperson.

3 thoughts on “The Connection Between Perimenopause and Stomach Issues”
Very informative.
Thanks
Thank you!
Thank you for another great article.