Experiencing diarrhea is uncomfortable and embarrassing. Unfortunately, digestive issues are common in menopause.
Table of Contents
ToggleThe good news is that diarrhea is manageable through diet and lifestyle. This article will discuss the causes and treatment options for diarrhea in menopause.
Diarrhea is passing loose, watery stools two or more times per day. In addition, you may also experience abdominal cramping, abdominal pain, bloating, nausea, fever, and vomiting (1).
Causes of Menopause and Diarrhea
Both menopause and non-menopausal reasons can cause diarrhea. Below are a few examples of each.
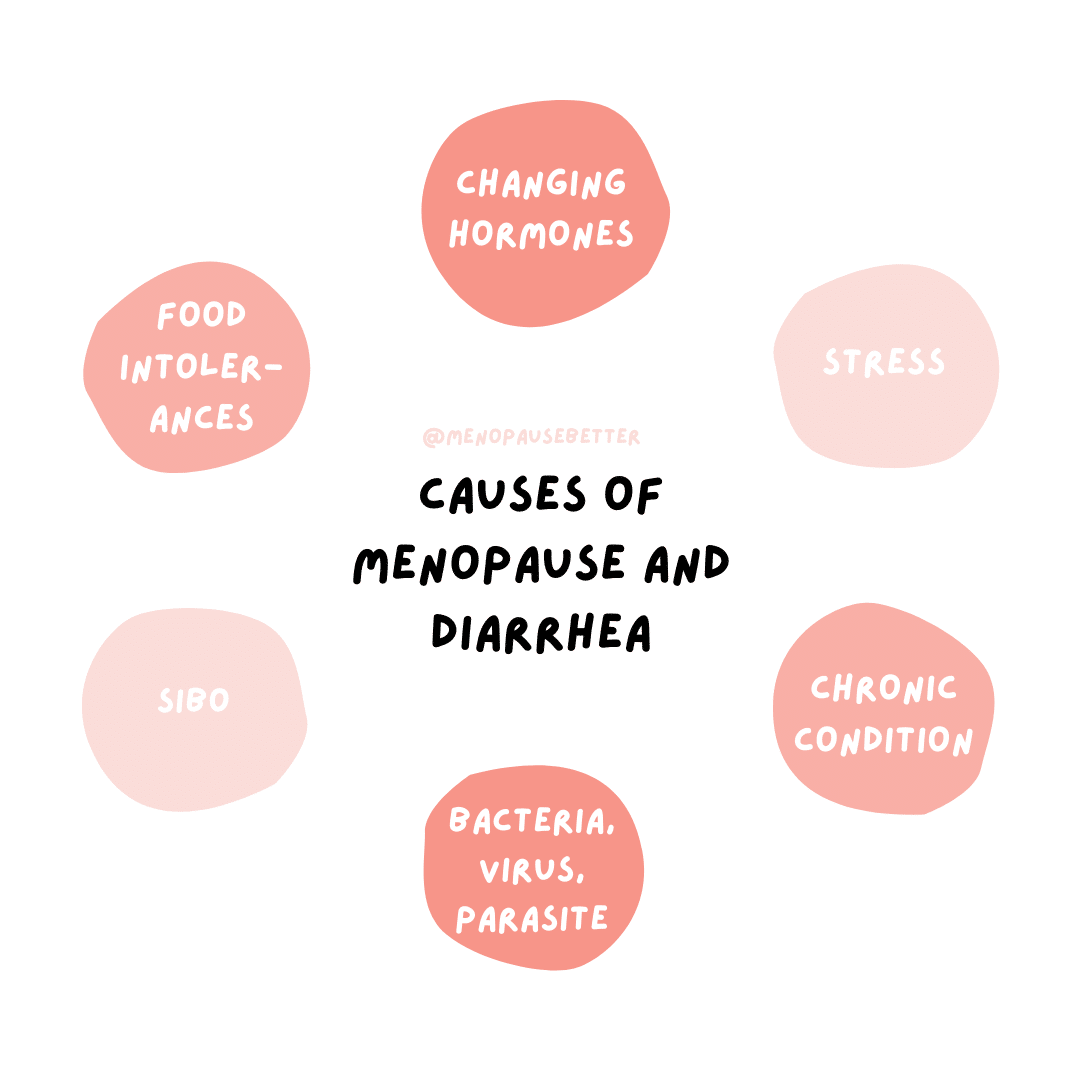
Changing Hormones
Changing sex hormones can affect gastrointestinal health.
For example, when progesterone hormone decreases, you may experience an increase in your bowel activity. This means food will move through your GI tract quickly, resulting in diarrhea.
Additionally, a change in hormone levels can lead to intestinal permeability. This causes diarrhea by irritating the lining of your digestive tract, weakening stomach muscles, or reducing absorption from food into the body (2).
Increased Stress
There is a well-known connection between stress the gut health. Stress on the nervous system can increase colonic motility and accelerate intestinal transit. As a result, you may experience diarrhea (3).
Menopausal women can have a stressful life between taking care of their children, aging parents, and professional careers. Furthermore, stress is also the result of an increase in cortisol, common in this age group.
Chronic Condition
Chronic diarrhea, or diarrhea lasting 6-12 months, is also common in menopause. However, chronic diarrhea may also indicate a more serious issue unrelated to menopause.
Chronic diarrhea is associated with irritable bowel syndrome (IBS), irritable bowel disease (IBD), celiac disease, and gallbladder problems (5).
Bacteria, Viruses, Parasites
Common bacteria, viruses, and parasites can cause chronic diarrhea.
For example, Giardia duodenalis (“Giardia”) is a common parasite that infects the intestines and causes diarrhea.
Giardia spreads from person to person or through contaminated water, food, surfaces, or objects. In fact, the most common way people get Giardia is by swallowing contaminated drinking water (6).
Small Intestinal Bacterial Overgrowth (SIBO)
Small intestinal bacterial overgrowth (SIBO) occurs when there is an abnormal increase in the overall bacterial population in the small intestine. These types of bacteria are not commonly found in the small intestine. As a result, a SIBO patient is likely to experience diarrhea (7).
Food Sensitivities & Intolerances
Lactose, fructose, sucrose, and FODMAP intolerances all result in chronic diarrhea. In addition, eating artificial sweeteners like mannitol and sorbitol also impact diarrhea. Last, eating spicy foods or caffeine may result in diarrhea (8).
Keep in mind that some women become more sensitive to specific foods as they enter menopause. So, if you are having diarrhea, place close attention to how your body reacts to different foods and remove those that trigger diarrhea.
Treatment for Menopause and Diarrhea
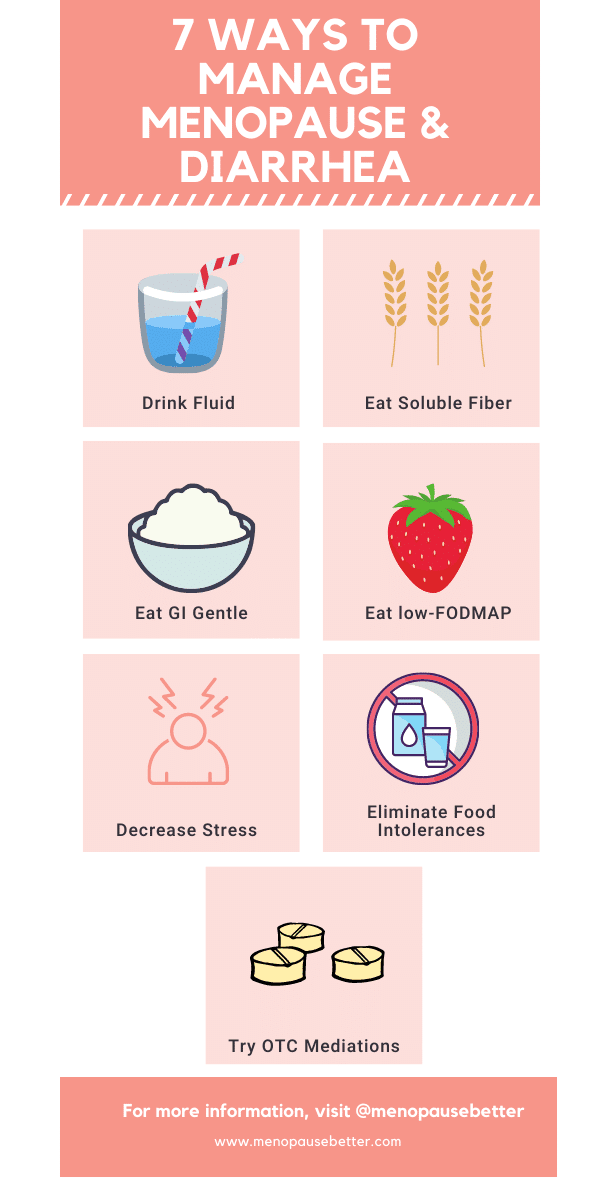
Drink Fluid
When you have diarrhea, you lose a lot of fluids in your body. It is important to replace those fluids. Therefore, drink plenty of liquids, including water, broths, and juices. Also, avoid dehydrating liquids like caffeine and alcohol (1).
Eat Soluble Fiber
Soluble fiber can help bind stools together, forming solid stools.
Foods high in soluble fiber include oats, beans, sweet potatoes, broccoli, carrots, pears, figs, nectarines, apricots, apples, flaxseeds, sunflower seeds, and hazelnuts (9).
GI Gentle Diet
If eating more soluble fiber doesn’t help, try the opposite approach by eating a low-fiber, low residue, low-fat diet. These foods include soda crackers, toast, eggs, rice, or chicken.
Additionally, avoid high-fat foods, dairy products, or highly seasoned foods for a few days (1).
Reduce Stress
Stress and gut health have a strong connection. When you experience chronic stress, there is a cascade of negative effects on your digestive system.
Thus, by managing stress, you can improve gut health while improving many other symptoms of menopause.
Focus on lowering cortisol levels and reducing stress in your life through high-quality sleep, exercise, participating in hobbies, and surrounding yourself with loved ones.
If possible, remove yourself from stressful home and work environments to improve stress (10).
Eliminate Food Intolerances
Foods that you tolerated well before now may be more difficult for you to digest. For example, gluten and lactose intolerance are common in many adults. Other foods difficult to digest include lactose, fructose, and sucrose.
So, be aware of what you eat, and if you notice that certain foods cause diarrhea, eliminate them for a few weeks (11).
Try a Low-Fodmap Diet
A low-FODMAP diet is 75% effective at reducing symptoms like diarrhea associated with irritable bowel syndrome. FODMAPs are short-chain carbohydrates that malabsorb in the small intestine, ferment in the colon, and produce uncomfortable GI symptoms like diarrhea.
IBS patients reduce diarrhea through avoiding common FODMAPs like wheat, lactose, garlic, onion, mango, and honey. It’s important to receive a diagnosis of IBS-D before starting this type of diet (12).
Medications for Menopause and Diarrhea
Depending on your symptom severity and diagnosis, you can take over-the-counter (OTC) and prescription medications for your diarrhea.
Over-the-counter (OTC)
OTC medicines can help you feel better if you have diarrhea. These are called anti-diarrheal medicines.
Anti-diarrheal medicines include: Imodium, Pepto-Bismol, and bismuth subsalicylate.
Don’t take OTC medications if bacteria or parasites are causing your diarrhea. Stopping diarrhea, in this case, can make your condition worse (1).
Probiotics
Good bacteria may help restore a healthy balance to the intestinal tract by boosting the level of good bacteria. Probiotics are available in capsule or liquid form and are also added to some foods, such as certain yogurt brands.
However, further research is needed to understand better which strains of bacteria are most helpful or what doses are needed (1).
Hormone Replacement Therapy
During menopause, your estrogen levels fall. Hormone replacement therapy or estrogen replacement therapy is an effective treatment for menopause. Balancing out estrogen may help regulate the digestive system, impacting diarrhea (13).
When to Call the Doctor
Speak with your doctor if your diarrhea is not going away or is getting worse.
Call your doctor right away if you have:
- Severe abdominal or rectal pain
- Blood in your stool
- Black, tarry stools
- High fever (greater than 101.3 F)
- Signs of dehydration
These can be warning signs of things like:
- Infection
- Inflammatory bowel disease (IBD)
- Pancreatitis
- Colon cancer
Your doctor will ask about your medical history, review your medications, conduct a physical exam, and order tests to determine the cause of your diarrhea.
Below are a few tests your doctor may run if you have severe diarrhea:
- Blood Test: A complete blood count test, measurement of electrolytes and kidney function tests to show the severity of your diarrhea.
- Stool test: Your doctor might recommend a stool test to see if bacteria or parasites are the cause of your diarrhea.
- Breath test: This type of test can help diagnose conditions like lactose intolerance or SIBO.
- Flexible sigmoidoscopy or colonoscopy: to diagnose conditions like irritable bowel disease.
- Upper endoscopy: to examine and biopsy the stomach and upper intestines and used to diagnose conditions like celiac disease (1).
Conclusion
While menopause is an expected part of a woman’s life cycle, the addition of diarrhea may come as a shock. Changes in estrogen and progesterone may lead to worsening diarrhea symptoms.
You can manage diarrhea through various natural remedies, such as diet, stress reduction, and OTC supplements.
Last, you should speak to your doctor and health care team if diarrhea is more severe.
“Menopause and Diarrhea” was written by soon-to-be Registered Dietitian Becky Rashidifard. Reviewed/edited by Su-Nui Escobar, DCN, RDN, FAND.

Dr. Su-Nui Escobar, a Registered Dietitian/Nutritionist in Miami, FL, is dedicated to empowering women in perimenopause and menopause to live healthier, more satisfying lives.
With a doctorate in clinical nutrition from the University of North Florida, she has expertise in menopause and weight loss, including the unique challenges faced by those on weight loss medications.
Su-Nui’s passion for her field is evident in her previous role as the Academy of Nutrition and Dietetics spokesperson.


6 thoughts on “Menopause and Diarrhea: Causes and Treatments”
Very factual and clear to understand
Thank you
Thank you! I hope it is helpful
Thank you very much for this article. I have seen a few doctors, had multiple tests over and over and nothing shows up. My IBS is out of control and I have had no possible answers until now. Thank you.
Thank you for the insight of the Menopause. This as helped me alot
I am very happy it was helpful 🙂
Thanks I have learn alot