Perimenopause and IBS: What You Need to Know
“Perimenopause and IBS” was written by Registered Dietitian Becky Rashidifard. Reviewed/edited by Su-Nui Escobar, DCN, RDN, FAND.
Table of Contents
ToggleIrritable bowel syndrome (IBS) is uncomfortable and embarrassing.
Perimenopause does not cause IBS but can make the symptoms worse. Often, perimenopausal women experience digestive issues that can contribute directly or indirectly to the condition.
IBS cannot be cured, but there is good news: most women can manage even acute gut issues through diet and lifestyle.
This article will discuss causes, symptoms, and treatment options in relation to perimenopause and IBS.
What is IBS?
IBS, or irritable bowel syndrome, is a disorder of the gastrointestinal (GI) system that specifically affects the large intestine. It’s not a rare condition; in fact, it affects millions of Americans.
IBS is a long-term problem that must be managed over time. Although the symptoms can be very uncomfortable and sometimes even debilitating, this disorder does not damage your intestines or increase the risk of colon cancer.
Symptoms of IBS
Women with IBS will experience some or all of these symptoms:
- Constipation
- Diarrhea
- Abdominal bloating
- Abdominal pain
- Cramping
- Gas
- Changes in bowel habits
- Changes in the appearance and texture of bowel movements
- Mucus in the stool

How Perimenopause Affects IBS
There are a few ways in which the transition to menopause and what comes after can affect irritable bowel syndrome.
Changes in Hormone Levels
Interestingly, receptors for sex hormones have been found in the intestines, suggesting that the GI is able to sense and react to them.
As women’s sex hormones are significantly affected by perimenopause, it naturally follows that women in this transition to menopause experience a variety of gastrointestinal symptoms, including worsening IBS symptoms.
Constipation and Diarrhea
Declining levels of progesterone and estrogen that women experience during this time slow gastrointestinal motility. As a result, food takes longer to get through your GI tract. The longer food remains in your digestive tract, the more water is reabsorbed back into your body. This results in hard stools and constipation.
Hormonal changes can also lead to gut permeability. This causes diarrhea by irritating the lining of your digestive tract, weakening stomach muscles, or reducing the absorption of nutrients from food into the body.
As a result, those being affected by diarrhea or constipation related to IBS can have their symptoms intensify during perimenopause.
Increase in Pain Sensations
Estrogen is associated with the production of serotonin, the feel-good hormone. During perimenopause, estrogen may drop, leading to a decrease in pain tolerance. As a result, abdominal pain associated with IBS may feel more painful.
Increase in Cortisol
In perimenopause, women’s levels of estrogen rise and fall erratically. So, not only can it decrease, but it can also increase as women approach menopause. An increase in estrogen can result in an increase in cortisol levels.
Cortisol is also known as the stress hormone, and it can contribute to the deterioration of IBS abdominal symptoms through changes in gut-associated immune tissue and the enteric nervous system.
Decrease in Bile Production
Low estrogen will also affect the production and flow of bile, a key factor for digesting fats. When you’re not producing enough bile, your gut has trouble breaking down fats, causing diarrhea.
For this reason, midlife women may be more sensitive to fat from food.
Increase in Sleep Disturbances
Sleep disturbances are common during perimenopause, and poor sleep is correlated to worsening IBS symptoms.
Inadequate sleep is due to fluctuating estrogen and progesterone levels, which leads to changes in cortisol and serotonin metabolism in the body. Both cortisol and serotonin impact the body’s sleep cycle.
Additionally, it is likely that a woman in perimenopause will experience night sweats, which also makes it difficult to sleep through the night.
Diagnosing IBS
A gastroenterologist provides an IBS diagnosis using the ROME IV criteria. Symptom severity varies, but IBS patients usually have symptoms for at least three months before getting diagnosed.
Diagnostic criteria:
- Related to defecation
- Associated with a change in frequency of stool
- Change in texture and appearance of stool
If you think you have IBS, it’s essential to go to the doctor and receive a diagnosis. Don’t be tempted to self-diagnose because your symptoms could be related to a more serious illness.
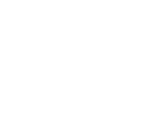
Treatment for Perimenopause IBS
There is a variety of ways to make a significant difference in how you experience IBS symptoms.
Change Fiber Intake
The right fiber intake can help manage GI symptoms. Judging the right amount is based on whether you’re suffering from constipation or diarrhea.
Constipation
An increase in fiber is recommended to meet current recommendations of at least 25g of fiber a day. Specifically, women with constipation will benefit from adding more insoluble fiber to their diet.
Insoluble fiber is found in whole grains, fruits and vegetables, nuts, and seeds.
Diarrhea
The type of fiber that dissolves in water helps form the stools. Therefore, women with diarrhea will benefit from adding more soluble fiber to their diet.
Soluble fiber is found in oats, legumes, flaxseed, and some fruits and vegetables.
Eat Smaller Meals
Eating smaller meals makes it easier for the digestive tract to do its job. Eating large meals can result in too much pressure on the digestive tract, and this pressure creates digestive issues.
For instance, be aware of potential tendencies to snack unnecessarily, eat in an undisciplined way from large buffets, or eat emotionally. It may help considerably to work on eating intuitively and acknowledging hunger and fullness cues.
Manage Fat Intake
When you have IBS, too much fat can cause diarrhea or constipation.
Women can reduce their fat intake in a few ways. For example:
- Cook food at home
- Reduce take-out food
- Decrease consumption of packaged foods
- Avoid fast food
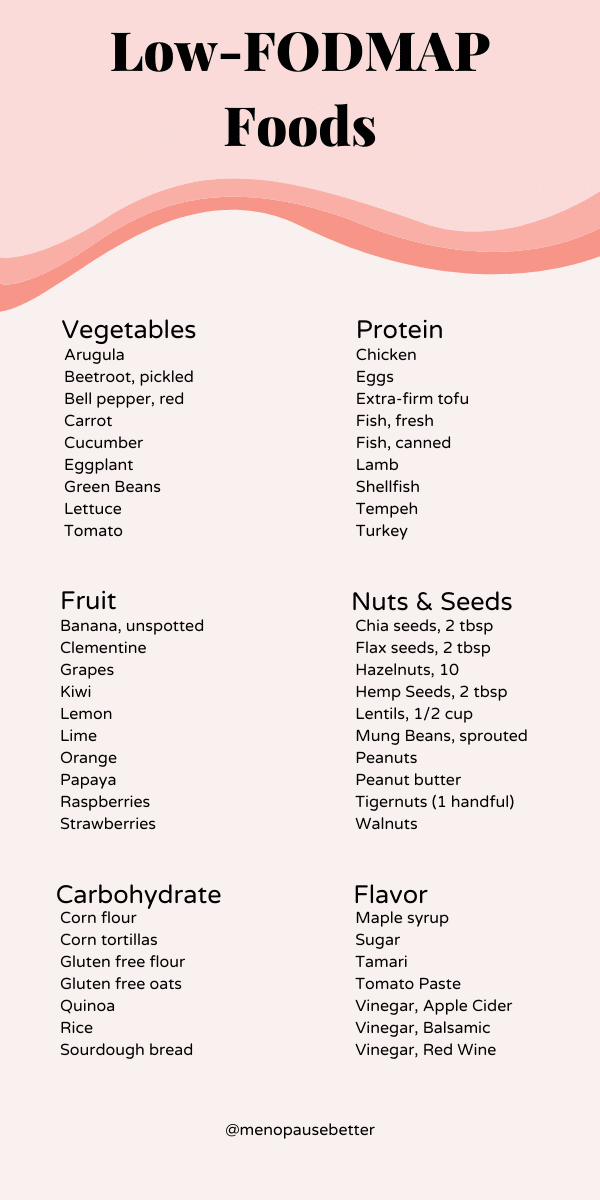
Adopt a Low-FODMAP Diet
The low-FODMAP diet, or the IBS diet, is 75% effective at reducing IBS symptoms.
What are FODMAPs? FODMAPs are a group of short-chain carbohydrates that aren’t absorbed properly in the gut, which can trigger symptoms in people with IBS. FODMAPs are found naturally in many foods, so it’s worth finding out what foods are high in FODMAPs when you suffer from IBS so that you know what to avoid.
Many common foods are high in FODMAPs, including garlic, onions, milk, wheat, shallots, leeks, asparagus, mangoes, apples, beans, high-fructose corn syrup, honey, cashews, and pistachios.
The FODMAP diet is a 3-step eating plan that includes an elimination, reintroduction, and personalization phase. By following this structure, you can pinpoint specific foods that worsen your IBS symptoms.
Visit Monash for more information and a complete guide to the low-FODMAP diet. It’s also a good idea to seek guidance from a Registered Dietitian who specializes in gastrointestinal health.
Decrease Stress
Stress and the resulting increased cortisol worsen IBS symptoms. What’s more, increased cortisol can also increase estrogen, making the triggers even more intense.
There are many ways to remedy stress and boost overall health. For example:
- Going on walks
- Spending time in nature
- Journaling
- Spending time with friends and family
- Playing with a pet
- Working on a hobby
- Yoga
- Pilates
- Mindfulness
- Talk therapy
- Massage therapy
Increase Exercise
Exercise is an excellent way to decrease stress and contribute to managing IBS symptoms. Research suggests that physical activity positively affects IBS symptoms and disease-specific quality of life, fatigue, depression, and anxiety.
It’s important to find a type of exercise you enjoy. For example, take a 30-minute walk, try yoga, pilates, run, or dance. The most important part of an exercise routine is consistently showing up.
Improve Sleep Quality
Poor sleep quality leads to worsening IBS symptoms, and perimenopause can worsen sleep quality. So you can see how perimenopause and IBS are interrelated.
Luckily you can improve sleep quality by making a few diet and lifestyle changes.
- Go to bed and wake up at the same time every day
- Stop using electronics at least two hours before bed
- Keep your bedroom at a cool temperature
- Wear sweat-wicking pajamas and sheets
- Keep your bedroom dark
- Avoid large meals before bedtime
- Avoid drinking alcohol
- Stop drinking coffee after midday
- Exercise during the day
- Stress less
Limit Alcohol
Limiting alcohol during perimenopause is a good idea for a variety of reasons.
First, drinking alcohol can increase estrogen levels, making IBS symptoms worse.
Also, alcohol disrupts the rapid eye movement (REM) phase, the part of sleep that’s the most restorative. Disruption of sleep leads to tiredness the next day, making you more likely to make poor health choices.
For instance, try replacing your nighttime wine or cocktail with a delicious mocktail, non-alcoholic beer, or a cup of warm caffeine-free tea.
Try Hypnotherapy
Hypnosis is a safe and effective treatment for managing IBS symptoms. There are several IBS-focused hypnotherapy apps that you can try.
Hypnotherapy can also improve hot flashes associated with perimenopause.
Medications for Perimenopause IBS
Diet and lifestyle choices may not be enough to manage IBS symptoms. For more chronic problems, other treatments available by prescription or over-the-counter are available.
It’s important always to discuss medication with your healthcare provider.
Over-the-Counter Medication for IBS
- Laxatives: increase transit time, relieving constipation and bloating
- Bulking agents: psyllium husk or bran can improve constipation, diarrhea, and bloating
Prescription Medication for IBS
Sometimes prescription medications are necessary for more severe IBS symptoms.
For example:
- Secretagogues/prosecretory drugs – increase fluid and movement in the GI tract.
- Anticholinergics/antispasmodics – relieve abdominal pain or discomfort after eating
- Anti-diarrheal drugs – slow gut transit and decrease diarrhea
- Anti-anxiety medication – relieve pain and improve the changes in bowel habit
- Antidepressants – reduce the intensity of pain signals going from gut to brain.
When to See a Doctor
Routine checks with your gastroenterologist are part of IBS management. However, there might be times when a visit to your general practitioner might be necessary between these visits.
It’s important to see a doctor if you experience the following symptoms:
- Weight loss
- Diarrhea at night
- Rectal bleeding
- Iron deficiency anemia
- Unexplained vomiting
- Difficulty swallowing
- Persistent pain that isn’t relieved by passing gas or a bowel movement
These symptoms can be signs of a more serious disease such as inflammatory bowel disease.
Summary
While perimenopause is an expected part of a woman’s life cycle, the addition of IBS symptoms may come as a shock.
The changes in estrogen and progesterone that come with perimenopause may worsen IBS symptoms, such as constipation, diarrhea, bloating, and pain.
IBS can often be managed at home through various natural remedies, such as diet changes, exercise, getting sufficient sleep, and reducing stress. A Registered Dietitian can help with these treatments. Additionally, you can speak to your doctor and healthcare team about taking prescription medication, if necessary.
References
Hale G. Faculty opinions recommendation of pain symptoms during the menopausal transition and early postmenopause. Faculty Opinions – Post-Publication Peer Review of the Biomedical Literature. 2010. doi:10.3410/f.5321957.5269055
Hypnosis for IBS. About IBS. https://aboutibs.org/treatment/complimentary-or-alternative-treatments/hypnosis-for-ibs/#:~:text=Hypnosis%20has%20been%20shown%20to,focused%20on%20the%20individual’s%20symptoms. Published May 16, 2022. Accessed August 15, 2022.
Ibs diet: What to do and what to avoid. About IBS. https://aboutibs.org/treatment/ibs-diet/ibs-diet-what-to-do-and-what-to-avoid/#:~:text=Eating%20stimulates%20the%20digestive%20tract,don’t%20rush%20through%20meals. Published May 13, 2022. Accessed August 15, 2022.
Irritable bowel syndrome – UNC school of medicine. https://www.med.unc.edu/ibs/wp-content/uploads/sites/450/2017/10/IBS.pdf. Accessed August 6, 2022.
Irritable bowel syndrome. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/irritable-bowel-syndrome/symptoms-causes/syc-20360016#:~:text=Irritable%20bowel%20syndrome%20(IBS)%20is,need%20to%20manage%20long%20term. Published December 1, 2021. Accessed August 6, 2022.
Johannesson E. Intervention to increase physical activity in irritable bowel syndrome shows long-term positive effects. World Journal of Gastroenterology. 2015;21(2):600. doi:10.3748/wjg.v21.i2.600
Kumar A, Saran K, Gupta R. Sleep disturbances and functional gastrointestinal diseases. Sleep and Neuropsychiatric Disorders. 2022:599-611. doi:10.1007/978-981-16-0123-1_29
Medications for IBS. About IBS. https://aboutibs.org/treatment/medications-for-ibs/. Published July 14, 2022. Accessed August 15, 2022.
Rome IV criteria. Rome Foundation. https://theromefoundation.org/rome-iv/rome-iv-criteria/. Published October 19, 2020. Accessed August 15, 2022.
Shieh A, Epeldegui M, Karlamangla AS, Greendale GA. Gut permeability, inflammation, and bone density across the menopause transition. JCI Insight. 2020;5(2). doi:10.1172/jci.insight.134092
Sugaya N, Izawa S, Saito K, Shirotsuki K, Nomura S, Shimada H. Effect of prolonged stress on the adrenal hormones of individuals with irritable bowel syndrome. BioPsychoSocial Medicine. 2015;9(1). doi:10.1186/s13030-015-0031-7
Sugaya N, Izawa S, Saito K, Shirotsuki K, Nomura S, Shimada H. Effect of prolonged stress on the adrenal hormones of individuals with irritable bowel syndrome. BioPsychoSocial Medicine. 2015;9(1). doi:10.1186/s13030-015-0031-7
“Perimenopause and IBS” was written by Registered Dietitian Becky Rashidifard. Reviewed/edited by Su-Nui Escobar, DCN, RDN, FAND.

Dr. Su-Nui Escobar, a Registered Dietitian/Nutritionist in Miami, FL, is dedicated to empowering women in perimenopause and menopause to live healthier, more satisfying lives.
With a doctorate in clinical nutrition from the University of North Florida, she has expertise in menopause and weight loss, including the unique challenges faced by those on weight loss medications.
Su-Nui’s passion for her field is evident in her previous role as the Academy of Nutrition and Dietetics spokesperson.